A 75 year old male presented with seizures
This is an a online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan.
Case.
A 75 year old male came to the casuality with chief complaints of seizures episodes since 3 years.
HOPI:
He was apparently asymptomatic 3 years back then he had his first episode of seizure which was abrupt lasted for 3 min
Then there was another episode of seizure which was 4 months back lasted for a period of 3-4 min.
Then there was another episode 4 days back which was abrupt, each episode of seizure is associated with bilateral upper and lower limb muscle spasms, uprolling of eyes, salivation along with teeth biting, confusion after the episode not associated with aura, tongue bite, involuntary defecation and micturition,sensory and motor deficits.
All these three episodes happened during sleep at night.
The patient was taken to the hospital after the first and second episodes for which he wasn't treated as he was not diagnosed.
Past history:
No significant history of seizures before 3 years.
Not a k/c/o diabetes, hypertension, TB, asthma, CAD.
History of fracture to femur which was immobilized with implantation a rod.
Personal history:
Diet - Mixed
Appetite - Normal
Bowel and bladder- Regular
Sleep- Adequate.
No known drug allergies
Addictions- H/o alcohol intake since 35 years 100 ml per day; last one year same of 100 ml per day on alternate days.
Alcohol last binge before a day of seizures
smoking beedi 1 packet since 35 years
General examination-
Patient is conscious, coherent, cooperative moderately built and nourished.
No pallor
No icterus
No clubbing
No koilonychia
No lymphadenopathy
No edema
Vitals-
Bp:. 170/110
PR : 93 beats/min
Spo2:96%
GRBS:145 mg/dl
Systemic examination-
CVS: S1 S2 +
RS:BAE+, NVBS+
P/A: soft, non tender
CNS:
Concious
Speech:normal
No neck stiffness
Cranial nerves, motor system, sensory system : NAD
Power Right Left
Upper limb 5/5 5/5
Lower limb 5/5 5/5
Tone. Right. Left
Upper limb Normal Normal
Lower limb Normal Normal
REFLEXES:
B T S K A P
RT. - - - - - M
LT. - - - - - M
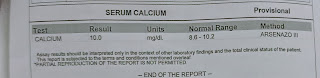
INVESTIGATIONS:
2D echo
CT scan
Day 2
1/12/21
ICU BED 1
S:
no seizure episode
No fever spikes
stools not passed
O:
Pt is conscious, coherent
Afebrile
PR-96bpm
Bp-140/90mmhg
Spo2-98 % RA
RR: 14CPM
GRBS: 82MG/DL
I/O: 800/600ML
CVS: S1S2+
R/S: BAE+
P/A: soft,non tender
CNS:
oriented to T/P/P
Pupils: NSRL
EOM: full
Speech: naming, repetition, comprehension +
Fluency decreased.
Power - 5/5 in all LIMBS
Tone - normal
REFLEXES:
B T S A K P
Right. - - 2+ - - Flexion
Left. - - 2+ - - Flexion
A:
GTCS SEIZURES secondary to
? ALCOHOL WITHDRAWAL.
P:
Inj thiamine100mg in 100ml NS i.v / TID.
Inj.lorazepam 2cc i.v/sos
Tab.levipil 500mg po/BD
Tab. Pan 40mg po/OD
Watch for seizure episode.
Temp charting
Monitor vitalsvitals 4th hrly.















Comments
Post a Comment