A 70 year old with shortness of breath.
This is an a online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan.This is an a online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
Maheshwari Jagathkari
Roll no 57
Case report
A 70 year old male carpenter by occupation came with chief complaints of
Shortness of breath since 1 week.
Anuria since 4 days.
Pain abdomen since 1 day.
HOPI
Patient was apparently asymptomatic 6 years back patient developed shortness of breath and was taken to the hospital and dialysis was done for about 3 times.
He was taking NSAIDS for his body pains since 20 years he stopped using the after dialysis was done.1 week back then he suddenly development shortness of breath of intially grade 4 for which he was taken to the some local hospital but the shortness of breath did not subside he was then taken to an another hospital where he also developed anuria since 4 days.bilateral pedal edema which is pitting type till the level below the knees, abdominal distension, facial puffiness since 2 days during his hospital stay.
There is no history of hesitancy, urgency, burning micturation.
Patient then developed pain abdomen which is diffuse, non radiating, dull aching type with no associating and reliving factors.
No history of fever, nausea and vomiting.
History of past illness
6 months back patient suffered left hemiparaesis of upper and lower limbs along with deviation of mouth to right, slurred speech and was resolved in 2 days when treated by a local doctor.
Daily routine
Patient wakes up at around 6 am in the morning then freshens up drinks tea and eats rice at around 10 am and eats directly at night at around 7 pm. During the day patient works and takes rest for 2 hours.
Past history
There is no history of diabetes, asthma, tuberculosis, coronary artery disease, epilepsy.
History of hypertension since 6 years.
Personal history
Diet is mixed with normal appetite and regular bladder movementsbut decreased urine output since 4 days, sleep is adequate.
Addictions
Patient used to smoke 5-6 beedis since the he was young and stopped 6 years back.
He used to take alcohol since he was young and stopped 6 years back.
No drug allergies.
No history of blood transfusion.
General examination
Patient is conscious, coherent and cooperative, well oriented to time, place and person, moderately built and nourished.
Pallor is present.
No features indicating the presence of pedal edema, icterus, cyanosis, clubbing, lymphadenopathy.
Vitals
Pulse rate 90bpm
Blood pressure 130/80mmhg
Respiratory rate 25cpm
Temperature - Afebrile
Systemic examination
CVS- S1 and S2 heart sounds heard, no murmurs.
RS- Bilateral air entry is present, normal vesicular breath sounds heard.
ABDOMINAL EXAMINATION
INSPECTION
No distention
No scars
Umbilicus - Inverted
Equal symmetrical movements in all the quadrants with respiration.
No visible pulsation,peristalsis, dilated veins and localized swellings.
PALPATION
No local rise of temperature
Abdomen is soft with no tenderness.
No spleenomegaly, hepatomegaly.
PERCUSSION
Liver span is 12cm.
No hepatomegaly
Fluid thrill and shifting dullness absent.
No puddle sign.
AUSCULTATION
Bowel sounds present.
No bruit or venous hum.
CNS examination
Higher motor functions intact
No focal neurological deficits.
Provisional diagnosis
Chronic kidney disease.
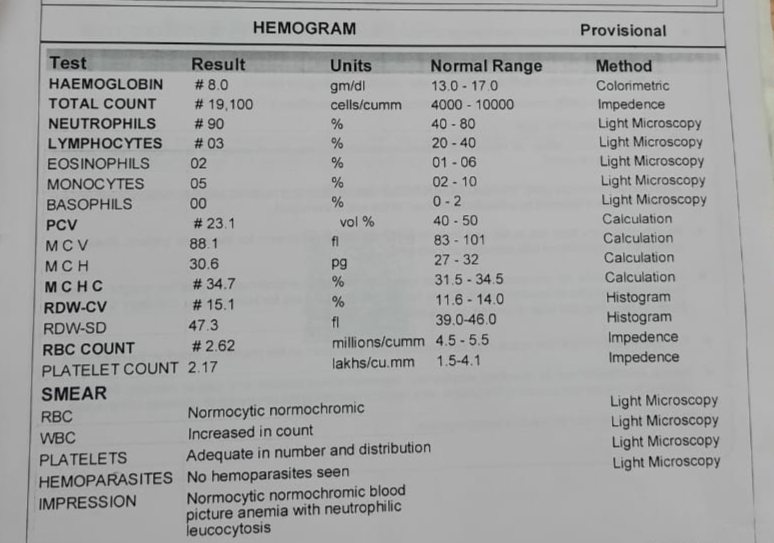
Investigations
CT links
https://youtube.com/shorts/iG_3ONeKjcw?feature=share
https://youtube.com/shorts/PnWU0ZIY5Nk?feature=share
Treatment
Day 9/8/22
Inj.lasix 80mg IV/stat
Inj.lasix 100mg 5mg/hr
Tab.Prazosin 5mg BD/PO
Tab.Met XL 50mg BD/PO
Tab.Nicardia 20mg BD/PO
Tab.Nodosis 500mg BD/PO
Tab.Rosuastatin 10mg + Tab.Clopidogrel 75mg OD/PO
Day 10/8/22
RT feeds 200ml milk + 100ml water
Tab.Nodosis 500mg RT TID
Tab.Nicardia 10mg RT BD (check BP before giving)
Inj.Lasix 40mg IV TID(if BP greater than 110/80)
Tab.Ecospirin 75/20mg RT OD
Inj.Pantop 40mg IV/OD
Tab.Orofer-XT RT/OD
Inj.Erythropoietin 4000IU sc twice weekly
Couse of illness.
Patient was intubated yesterday morning in the view of severe respiratory distress and falling SPO2 and was taken up for one session of dialysis in the view of renal failure.
Patient had sudden cardiac arrest at 6 pm, revived after 2 cycles of cpr.
Again suffered an arrest at 1 am and could not be revived.













Comments
Post a Comment